Patient procedures
Orthopaedic surgery complications
EARLY COMPLICATIONS
Every surgical procedure involves risks; the presence of associated diseases can increase these risks. The main complications related to joint replacement surgery are the following (this list is not exhaustive):
There is blood effusion in the joint (haemarthrosis) or the formation of a haematoma. This effusion might be minor and relieved by applying ice on the operated limb. If it is excessive, needle aspiration or even a surgical procedure, might be required to evacuate it.
This risk is prevented by careful vascular coagulation during the procedure, by the placement of drains when the surgical wound is being closed (to pull up and evacuate blood) and with the use of a compressive bandage. This complication is rare in the hip and somewhat less rare in the knee.
On the contrary, ecchymosis (blue colouring of the skin) is common.
This is a rare but serious complication that often requires a repeat procedure (to clean the operated joint and sometimes change the implant) and long-term antibiotic treatment. Infection can occur early after the procedure and in this case, is due to contamination of the operating site, usually by the skin.
Infection prevention measures are implemented from the moment you are hospitalised, along with hygiene teaching.
An infection can occur later on, due to a germ transported by the blood. There are certain factors that contribute to infection: immunomodulatory treatment that weakens the body’s defence mechanisms (chemotherapy, disease-modifying drugs for rheumatoid arthritis, etc.), long-term use of corticosteroids, diabetes, and obesity.
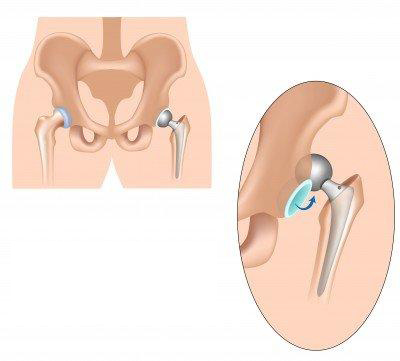
Dislocation of the implant is a complication that can occur during an incorrect movement (especially during the first three months after the procedure), when the muscles surrounding the implant are too weak. This complication mostly applies to hip replacement implants. To prevent this complication, it is important to avoid certain movements, especially during the first three months after the operation. This is why the physiotherapists teach you the required precautions during your hospital stay.
Phlebitis (inflammation of a vein) can become complicated a venous thrombosis (clot in the vein). Immobilisation contributes to it. A fragment of the clot can sometimes detach and migrate to the lungs: this is a pulmonary embolism. The risk of thrombosis is now rare because of exercises to stimulate venous return in the legs, early mobilisation, anticoagulant treatment (that thins the blood) starting on the day before the procedure, and wearing support stockings.
This can occur when the implant is being placed: this is also a very rare complication that is due to bone fragility. This complication can make placement of the implant somewhat more difficult.
This is a very rare complication that affects the nerves located close to the implant, which can be harmed during the implantation procedure. Usually the paralysis regresses, but recovery can take several months.
LATE COMPLICATIONS
This invariably occurs for all implants and causes the implant to loosen. Loosening of the implant (loss of fixation of the components) manifests itself through pain and migration of the implant components; it requires a revision.
This occurs either via the blood from an infectious focus (skin, urine, bronchi, vesicle, sinus, etc.) or is due to a surgical contamination that went unnoticed, that develops silently and can lead to septic loosening of the implant.
This is rare. The bone that could form around the total hip replacement implant after the procedure could result in joint stiffening. This is prevented by the systematic use (except in the case of a specific contraindication) of non-steroidal anti-inflammatory drugs for a few days after the procedure. This complication mainly affects hip replacement implants.
This can occur with certain implants, such as in the knee, elbow or shoulder. This is due to the presence of adhesions that limit mobility (the soft tissues are "stuck" together). It can be prevented by early gentle mobilisation of your implant, passive mobilisation or with the use of a machine.
This is a "deregulation of the nervous system that controls the vessels" and it causes pain, swelling and can result in stiffening of the joint. It is a complication that occurs and develops in an inconsistent and unpredictable way. Treatment is based on a combination of medicines and gentle specialised rehabilitation. The progression can be over several months.
There is swelling in the replacement joint, especially in the knee, which can require a puncture to verify the absence of infection. Specific local actions can be discussed and carried out in agreement with the surgeon in a specialised service, to dry out the effusion (isotopic synoviorthesis).
This can occur long after the procedure: if you are experiencing pain in a calf, or are out of breath, please consult your physician.